Concussions result in microscopic white matter and inflammatory changes to the brain, say three new studies.1-3
The studies, published in the Journal of Neurosurgery, said co-lead author, Dr. Paul Echlin of the Elliott Sports Medicine Clinic in Burlington, Ontario, Canada, "contribute to converging objective evidence concerning the acute and chronic effects of repetitive brain injury in the sports."
They add to a growing body of research suggesting that concussion can no longer be thought of as a transient injury resulting in just a temporary disruption of brain function, but that it results in persistent structural and electrophysiological changes as well.
Vascular changes
In the first study,1 researchers used a relatively new MRI modality called susceptibility-weighted imaging (SWI) to measure small changes in the brain called hypointensities in a group of adult male and female adult hockey players in Canada.
They found statistically significant change in hypointensity burden (HIB) in concussed males and a smaller non-significant increase in concussed females three days after concussion, which peaked at two weeks post-injury but returned to preseason levels by season's end. Such hypointensities are thought to be subtle signs of chronic and acute damage due to both subconcussive and concussive injury.
The researchers were unable to account for the gender difference, but speculated that it may have been due to the fact that every individual in the concussed group of male subjects had suffered previous concussions, while a lesser number of the female hockey players had a history of concussions, and perhaps also to a greater tendency of males to underreport concussions.
Although the vascular effects went away, it was "not clear if that would be the case in people who suffer multiple concussions over a period of years," noted study author Ofer Pasternak, a researcher at Brigham and Women's Hospital, in an interview with CTV News in Canada.
And we [also] don't know whether the changes in vascular properties would be affecting other types of changes in the brain that would persist for a longer time," he said.
"Given what is known about the occurrence of multiple subconcussive blows and later concussions, [SWI] may be useful in the detection of cumulative effects of concussion," the study concludes.
White matter changes
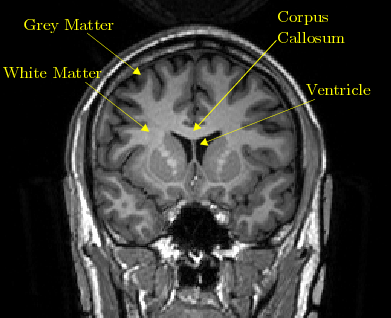
In the second study,2 researcher used an advanced form of imaging called Diffusion MRI or dMRI to detect microstructural alterations after concussion to the white matter of concussed players' brains, which are the long tissue fibers through which messages pass between different areas of gray matter within the brain and spinal cord, likened to the cables that connect individual computers in a network.
"What we think we see is some kind of immune response that is activated right after the concussion," Pasternak told CTV News.
"We cannot say yet whether it is long-term damage," although such changes might contribute to long-term neurological deficits or to degenerative diseases such as chronic traumatic encephalopathy, or CTE, in the future," he said.
Structural changes persist
In the final study,3 researchers compared the scans of concussed players' brains with non-concussed athletes using an advanced imaging technique called Diffusion Tensor Imaging (DTI) and found changes in white-matter microstructure in those with a history of concussion which were still evident on the end-of-season scan.
The researchers weren't sure why such alterations of the brain's white matter microstructure occurred, but speculated that it may reflect neuroinflammatory or neuroplastic processes of the brain responding to trauma.
They also said it was too early to tell what the long-term effects are.
Caution ahead
Martha Shenton, director of the psychiatry neuroimaging laboratory at Brigham and Women's Hospital and co-principal author with Dr. Echlin on the studies, urged caution in interpreting the results.
"I think one has to be careful here and not say, 'Hey, we're showing permanent damage,"' Shenton told CTV News.
"We aren't saying that. We're saying there's evidence of changes here and we don't know whether they're going to be long term or whether they're going to resolve and what they're associated with."
"But it's at least a little kind of warning ... that if someone has a concussion, don't send them back (to play) right away, give them the proper rest period they need before they get a secondary impact, which can actually be fatal," she stated.
"We know that trauma occurs. We know that in soft tissue you're going to have these findings of inflammation and neuroplasticity, which means changes in the structure, but we'd never seen it before," said Dr. Echlin in the CTV News interview.
The authors stressed that the findings were important, not just for hockey but for football and soccer players, or indeed for anyone who suffers a concussion or mild traumatic brain injury.
Society's choice
The studies are the latest research from by the Hockey Concussion Education Project (HCEP), a collaboration between Echlin and researchers at the Harvard Medical School, Brigham and the Women's Hospital, and Massachusetts General Hospital in Boston, and at the Athinoula A. Martinos Center for Biomedical Imaging in Charlestown, MA, and the Western University of Canada,
Along with previous peer-reviewed studies by HCEP published 20104-7 and 2012,8-14 Echlin said they provide "clear evidence of microstructural and hemodynamic alterations that occur following concussion."
His hope is that the studies "will help increase the awareness of the possible results of concussions and in this way act as an enticement for future participation in similar studies. We expect that with a larger sample the methods described here may identify additional microstructural alterations that occur following a concussion."
In the end, Echlin said, what is done depends on society's goals: "Will we foster the development of our young people's cognitive, social and physical potential in a safe and protected environment - or will we continue to teach and reward a culture of violence and accepted brain injuries as "part of the game'"? Are we able to evolve and make significant or even radical changes in the sports themselves based on the scientific evidence of too many serious short and long-term brain injuries?"
Sources:
1. Helmer KG, Pasternak O, Fredman E, Preciado RI, Koerte IK, Sasaki T, Mayinger M, Johnson AM, Holmes JD, Forwell LA, Skopelja EN, Shenton ME, Echlin PS: Hockey Concussion Education Project, Part 1. Susceptibility-weighted imaging study in male and female ice hockey players over a single season. J Neurosurgery 2014; DOI: 103171/2013.12.JNS132093 (published online, ahead of print, February 4, 2014)
2. Pasternak O, Koerte IK, Bouix S, Fredman E, Sasaki T, Mayinger M, Helmer KG, Johnson AM, Holmes JD, Forwell LA, Skopelja EN. Shenton ME, Echlin PS: Hockey Concussion Education Project, Part 2. Microstructural white matter alterations in acutely concussed ice hockey players: a longitudinal free-water MRI study. J Neurosurgery 2014; DOI: 103171/2013.12.JNS132090 (published online, ahead of print, February 4, 2014).
3. Sasaki T, Pasternak O, Mayinger M, Muehlmann M, Savadjiev P, Bouix S, Kubicki M, Fredman E, Dahlben B, Helmer KG, Johnson AM, Holmes JD, Forwell LA, Skopelja EN, Shenton ME, Echlin PS, Koerte IK: Hockey Concussion Education Project, Part 3. White matter microstructure in ice hockey players with a history of concussion: a diffusion tensor imaging study. J Neurosurgery 2014; DOI: 103171/2013.12.JNS132092 (published online, ahead of print, February 4, 2014)
4. Echlin PS. Editorial. Concussion education, identification, and treatment within a prospective study of physician-observed
junior ice hockey concussions: social context of this scientific intervention. Neurosurg Focus 2010;29(5):E7
5. Echlin PS, Johnson AM, Riverin S, Tator CH, Cantu RC, Cusimano MD, et al. A prospective study of concussion education
in 2 junior ice hockey teams: implications for sports concussion education. Neurosurg Focus 2010;29(5):E6, 2010
6. Echlin PS, Tator CH, Cusimano MD, Cantu RC, Taunton JE, Upshur REG, et al: A prospective study of physician-observed
concussions during junior ice hockey: implications for incidence rates. Neurosurg Focus 2010;29(5):E4
7. Echlin PS, Tator CH, Cusimano MD, Cantu RC, Taunton JE, Upshur REG, et al. Return to play after an initial or recurrent
concussion in a prospective study of physician-observed junior ice hockey concussions: implications for return to play after a concussion. Neurosurg Focus 2010;29(5):E5.
8. Echlin PS, Grady MS, Timmons SD. Introduction: Concussion: pathophysiology and sequelae. Neurosurg Focus 2012; 33(6): Introduction. DOI: 10.3171/2012.10.FOCUS12357.
9. Echlin PS. Editorial: A prospective study of physician-observed concussion during a varsity university ice hockey season. Part 1 of 4
Neurosurg. Focus 2012;33(6): E1; DOI: 10.3171/2012.9.FOCUS12287.
10. Echlin PS, Skopelja EN, Worsley R, et al. A prospective study of physician-observed concussion during a varsity university ice hockey season: incidence and neuropsychological changes. Part 2 of 4. Neurosurg. Focus. 2012;33(6): E2, DOI: 10.3171/2012.10.FOCUS12286.
13. Koerete IK, Kaufmann D, Hartl E, et al. A prospective study of physician-observed concussion during a varsity university hockey season: white matter integrity in ice hockey players. Part 3 of 4. Neurosurg. Focus 2013;33(6):E3; DOI: 10.3171/2012.10.FOCUS12303.
14. Chamard E, Théoret H, Skopelja EN, et al. A prospective study of physician-observed concussion during a varsity university hockey season: metabolic changes in ice hockey players. Part 4 of 4. Neurosurg. Focus 2012;33(6):E4. DOI: 10.3171/2012.10.FOCUS12305.
Additional material from a Hockey Concussion Education Project Media Advisory dated February 4, 2014 was used in the preparation of this article.








