A 2013 study linking frequent heading of a soccer ball with changes to the white matter of the brain and poorer performance on a neurocognitive test of memory [1] added fuel to the fire of a 30-year-old debate about the effects of heading.

The study by researchers at the Albert Einstein College of Medicine in New York is believed to be the first to quantify subconcussive heading and to assess the association of heading with imaging evidence of brain injury and impaired neurocognitive function.
The findings suggest that may be a heading threshold above which the risk of short- and possibly long-term brain injury dramatically increases.
Establishing such thresholds, the scientists say, could ultimately lead to identification of a 'head count' above which a player's heading should be curtailed for a specific recovery period, an approach akin to the pitch counts implemented in youth baseball to reduce the risk of arm injuries, and an approach that has been proposed by some concussion experts as a way of reducing the risk of long-term brain injury from subconcussive impacts in contact and collision sports.
Study details
Researchers at Albert Einstein College of Medicine in New York studied a group of 37 adult, mostly male amateur soccer players, who had been playing soccer for an average of 22 years and reported having played an average of 10 months in the past year, during which they reported heading between 32 and 5,400 times (median of 432).
Looking for subtle signs of traumatic brain injury (TBI) from repetitive soccer heading, they scanned the brains of players using an advanced MRI technique called diffusion-tensor-imaging (DTI) which spots microscopic changes in the white matter of the brain (the long tissue fibers through which messages pass between different areas of gray matter within the brain and spinal cord, likened to the cables that connect individual computers in a network), and had them take a computerized neurocognitive test looking for effects on cognitive function. Their hypothesis was that a threshold for heading exposure would be detectable, above which its association with imaging and neurocognitive abnormalities would significantly increase.
What they found were four different heading thresholds: three (at 885, 1291, and 1558 heads, respectively) above which heading significantly increased the statistical risk of abnormalities in the three different areas (what they called "regions of interest" or ROI) of the white matter of the brain on a DTI measure called fractional anisotropy (FA), and a fourth, higher thresh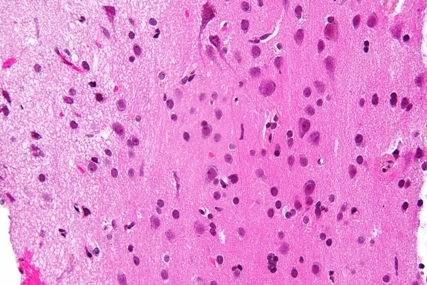 old (1798 heads) linked to poorer neurocognitive performance on a computerized neurocognitive test of memory. Their findings were not significantly associated with prior concussion, yet consistent with findings seen in patients with TBI.
old (1798 heads) linked to poorer neurocognitive performance on a computerized neurocognitive test of memory. Their findings were not significantly associated with prior concussion, yet consistent with findings seen in patients with TBI.
'Intriguing clues'
"The relationships detected in this current study ... provide some intriguing clues to pathophysiologic mechanisms," according to the lead author, Michael L. Lipton, MD, PhD, and his Albert Einstein colleagues. "It is well established that most patients with mild TBI recover fully over time, indicating that intrinsic mechanisms [in the brain] are generally able to effect repair of low-level injury. ... Increasing heading exposure up to a threshold, without associated imaging or cognitive changes, may indicate a range of exposure within which these intrinsic injury repair mechanisms are effective. The appearance of significant associations of imaging and cognitive changes with heading above the threshold, on the other hand, suggests that these repair mechanisms may be unable to keep pace with the cumulative injury that occurs beyond this degree of exposure."
Lipton and colleagues said that their findings of lower heading thresholds for increased risk of abnormal changes to the three ROI in the brain and a higher threshold for impaired memory function were expected, and likely reflected a widely recognized epidemiologic phenomenon in which tissue damage precedes damage that impairs day-to-day functioning, and which can be detected on clinical examination without the use of sensitive measures such as DTI or neurocognitive tests.








