To further the integration of athletic training within the public health arena, athletic trainers need to expand their professional focus from the teams and athletes they work with at their institutions to all physically active individuals, urged the National Athetic Trainers' Association at a press conference at its 2016 Clinical Symposia and AT Expo in Baltimore, Maryland and in a report on its Athletic Training and Public Health Summit published in the Journal of Athletic Training. (1)
"The most pressing health problems facing active children and adults require population-based approaches to reduce or prevent injury," says lead author Mark Hoffman, PhD, ATC, vice provost for international programs, Oregon State University. "We held a summit that included three symposiums in August 2015 to address this topic and explore opportunities for athletic trainers and others to partner with public health professionals and identify clear steps for change."
The Centers for Disease Control and Prevention Foundation defines public health as the "science of protecting and improving the health of families and communities through promotion of healthy lifestyles, research for disease and injury prevention and detection and control of infectious diseases." Public health approaches emphasize prevention over treatment, populations over individuals, and engagement at multiple levels.
The objectives of the summit were to: 1) describe the benefits of using a population-based approach to address concerns; 2) identify specific skill sets and potential partnerships that would be beneficial for maximizing the prevention of injuries and illnesses; and 3) identify and develop potential solutions to challenges that arise in the development, translation, adoption and assessment of preventive policies, guidelines and practices.
Public health approach to sports safety urged
Participants followed a process commonly used to address health problems:
- describe the magnitude of the problem (incidence and burden);
- identify risk factors and mechanisms;
- develop interventions for the risk factors identified;
- assess the efficacy and effectiveness of the intervention to reduce incidence;
- describe the intervention context to understand what can actually be implemented in real-world settings; and
- implement and evaluate the effectiveness of interventions.
The summit focused on three types of prevention:
- Primary prevention: which focuses on interventions before the injury or illness has happened (e.g., neuromuscular programs to prevent knee injuries);
- Secondary prevention: which focuses on intervention immediately after injury or illness has happened (early treatment, slowing of disease); and
- Tertiary prevention: which focuses on improving outcomes for those with long-term injuries or illnesses (e.g., knee or ankle osteoarthritis).
"It is critical for athletic trainers and others to understand the impact they can have on public health and identify specific areas of clinical practice. Similarly, policy development and assessment are two fundamental aspects of public health that are highly applicable to a wide variety of health care professions as they pertain to injury prevention and safety in the workplace or on the athletic field," says Hoffman.
Three Areas of Focus
The summit focused on three important areas of sports injury prevention:
1. Sudden Cardiac Death and Development and Implementation of Policies and Guidelines for Injury Prevention
Sudden cardiac arrest is the most common cause of death in high school and college athletes:
- 2,000 children in the U.S. die every year from sudden cardiac arrest.
- Sudden cardiac arrest (SCA) is the leading cause of death in exercising young athletes.
- Approximately one in 300 young athletes has a heart disorder that may increase his or her risk of sudden cardiac arrest.
Speakers addressed challenges of screenings in different sports settings and the need to engage stakeholders and establish polices. They recognized that a "one-size-fits-all" approach to cardiac screenings may not be appropriate for all athletic populations, and highlighted the existing challenges and controversies associated with implementing cardiac screening in settings ranging from the National Football
League to high school basketball.
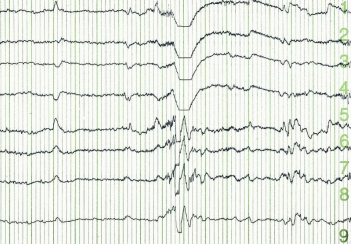
2. Sport-Related Concussion and Program and Policy Evaluation
Sports-related concussions are a serious public health concern, with some suggesting that the numbers have reached epidemic proportions. Studies show that:
- There are three times as many catastrophic head injuries in football among high school athletes than college athletes, and that 39 percent of the athletes were playing with symptoms from a prior head injury.
- According to the Centers for Disease Control, 163,670 young athletes were seen for a concussion in the emergency department of U.S. hospitals in 2012, representing more than 8 percent of the 1.35 million youth sports-related injuries seen in emergency rooms, which equates to a child being seen every three minutes in an ER for a sports-related concussion.
- Among high school athletes, concussion rates have risen 200 percent in the past decade.
Since the first concussion law went into effect in May 2009, all 50 states have adopted so-called Lystedt Laws. The effect of such legislation has not been widely studied, but a 2014 study by researchers at the University of Michigan (2) designed to evaluate the impact of the new concussion laws found a 92 percent increase in children seeking medical assistance in states with such legislation in place compared to a 75 percent increase in states without concussion laws.
While recognizing that the increase in the incidence of concussion may be due to increased awareness, the speakers nevertheless encouraged rigorous evaluation of policies to fill safety gaps (many non-school-sponsored activities are not covered by state law) and too many schools still do not have an athletic trainer on staff.
3. Osteoarthritis and Translation to Practice
Acute traumatic knee joint injuries are common in young athletic populations, which significantly increase the risk for posttraumatic osteoarthritis. Guidelines exist, note the authors, but need to be disseminated and implemented.
- According to the CDC, osteoarthritis affects 13.9 percent of adults in the United States aged 25 years and older and 33.6 percent (12.4 million) of those 65 and older: a total estimated 26.9 million U.S. adults.
- Who needs to be involved in the discussions moving forward?
- What skills, knowledge and abilities do athletic trainers or others need in order to see their work through a public health lens?
- What educational opportunities and activities will promote the integration of athletic training and public health?
- In what areas are athletic trainers (and other health care professionals) already taking the lead in public health-related initiatives and in what other potential areas may athletic trainer expertise and public health- related initiatives overlap?
Source: National Athletic Trainers' Association
1. Hoffman M, Bovbjerg V, Hannigan K, Hootman JM, Johnson STG, Kucera KL, Norcross MN. Athletic Training and Public Health Summit. J Athl Tr. 2016;51(7):000-000 doi: 10.4085/1062-6050-51.6.01 (e-pub ahead of print, June 23, 2016)
2. Gibson TB, Herring SA, Kutcher JS, Broglio SP. Analyzing the effect of state legislation on health care utilization for children with concussion. JAMA Pediatr. 2015;169(2):163-168. doi:10.1001/jamapediatrics.2014.2320.
Posted June 23, 2016








